NETWORK – Globalhealth
Information for Physicians

Faculty of Keloid
Information on the therapy of Intralesional Cryosurgery of keloids and the procedure
Search for doctors
If you are looking for a certified doctor, follow this link:
Search for doctors
Patient information
Attention! This page is intended for doctors!
Patients, who would like to inform themselves about the therapy, please visit the patient information to this topic: LINK
Note for physicians
The information provided here is in no way a substitute for training in how to carry out the therapy.
A certification to administer the therapy is required. Please contact us if you are interested.
Topic navigation
Department Keloid is pursuing the introduction of Intralesional Cryosurgery (IC) for the treatment of keloids – also in the interest of many patients. Intralesional cryosurgery has a recurrence rate of only 5-7% for most keloid types. It can be combined well with all therapies used so far.
The therapy
The treatment of keloids has always been an unsatisfactory duty for physicians. The overproduction of altered collagen fibres and the overexpression of TGFβ, which stimulates the uncontrolled growth of a sometimes small injury, has been successfully treated in some cases, but the predictability of long-term outcomes has been virtually impossible. Recurrence rates are extremely high or the procedures used have brought other serious disadvantages for patients. Intraläsional cryosurgery now provides us with a therapeutic procedure that allows improved predictability of results for at least some keloid types.
The procedure
The development of the method is the result of an Israeli-German cooperation between the working groups of Prof. Dr. Yaron Har-Shai, Haifa and Prof. Dr. Christos C. Zouboulis, Berlin (currently Dessau). Both working groups independently produced a special needle for intralesional cryosurgery. After a 6-month collaboration at Freie Universität Berlin, it was decided to further develop the special needle manufactured in Israel, which is closed at the front.
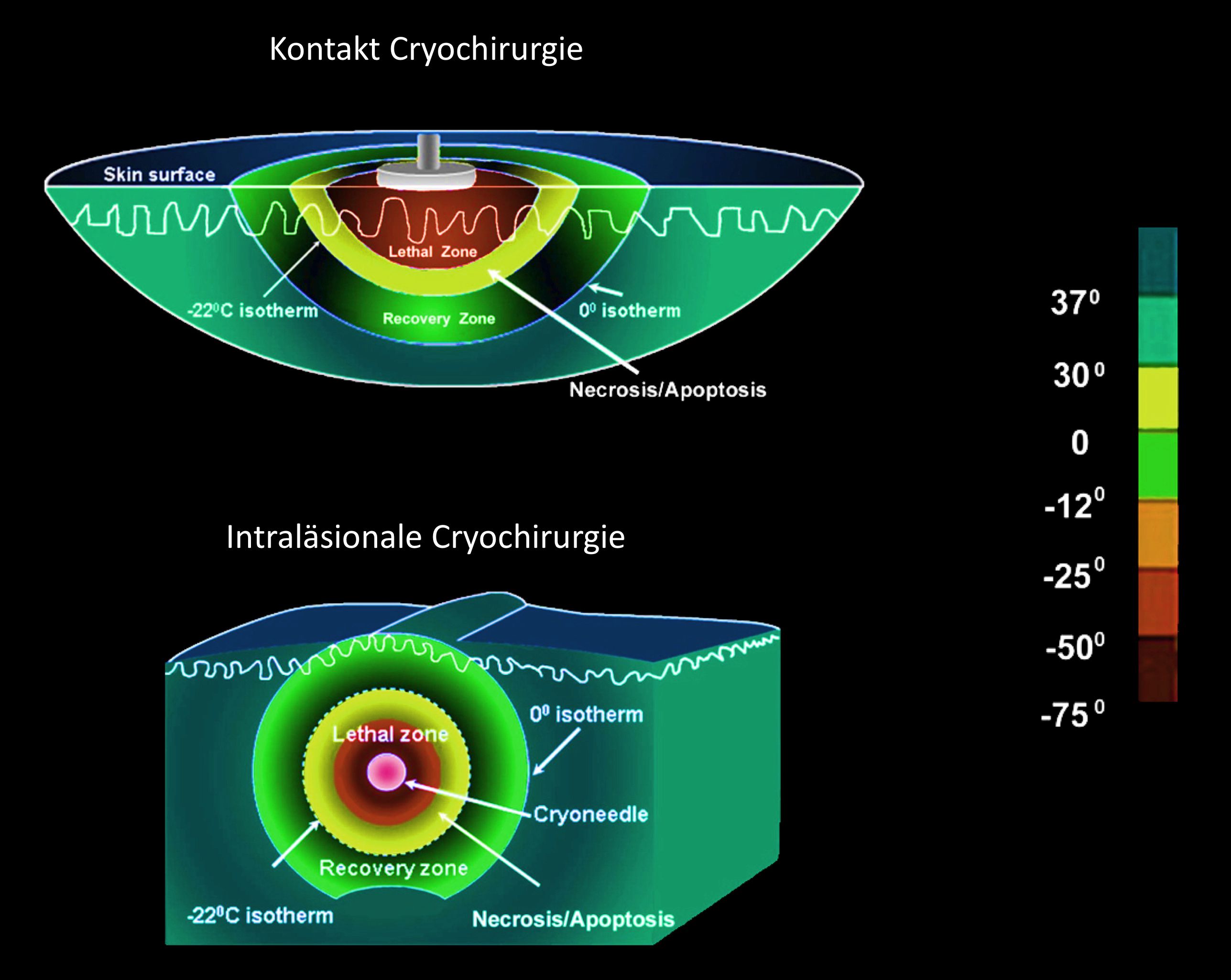
The nitrogen introduced circulates continuously through the needle and is then discharged again. As a result, constant temperatures of about 2 cm in diameter around the needle (length: 10 cm) can be found at the site of the needle. These temperatures are so low (-40°C) that the number of cold-resistant fibroblasts is reduced and collagen fibers are destroyed. The needle is placed in the lower third of the keloid. If the keloid has a width or depth greater than 2 to 3 cm, the needle must be inserted several times in succession to freeze the whole tissue. For dermatologists who are familiar with spray or contact cryosurgery, the duration of the passage takes getting used to. It is not calculated in seconds, but the application takes considerably longer, starting with at least about 10 minutes, and can even last up to more than 60 minutes, depending on the size of the keloid and the vascularization of the tissue.
As a standard it is stated that in healthy tissue a lighter discoloration in a width of 2 to 10 mm around the keloid must be visible, a so-called halo (Fig. 1), only then can the treatment be completed.
The CryoShape® needle is usually inserted under local anesthesia. Approximately one hour before treatment begins and 3 to 4 hours after treatment, painkillers can be administered to the patient. A few hours after the treatment, a weeping bladder forms which crusts within 8 to 10 days (Fig. 2a-d). The bladder roof contains antibiotic peptides and should not be removed to prevent wound infections. The treated keloid should be re-bonded once a day. During the first 7 days, a steroid cream should be applied daily to the lesion to reduce swelling and secretion from the treated lesion. A silicone or fat film should be applied between the bladder roof and the dressing until the wound has dried out.
The treated keloid continues to degenerate and the result can be assessed after 6 months. The skin still shows signs of the former keloid, but the increase can decrease significantly to almost disappear. Even the symptoms of itching and pain, which are very unpleasant for patients, no longer occur or are greatly reduced within a week after the treatment (Fig. 3).
Publications
The first investigations were carried out in Israel and Germany. Many parameters were examined which helped the new therapy to present meaningful study results. In detail, the temperature conditions around the needle, on the keloid surface and in the surrounding healthy tissue were investigated.
Many positive effects were found:
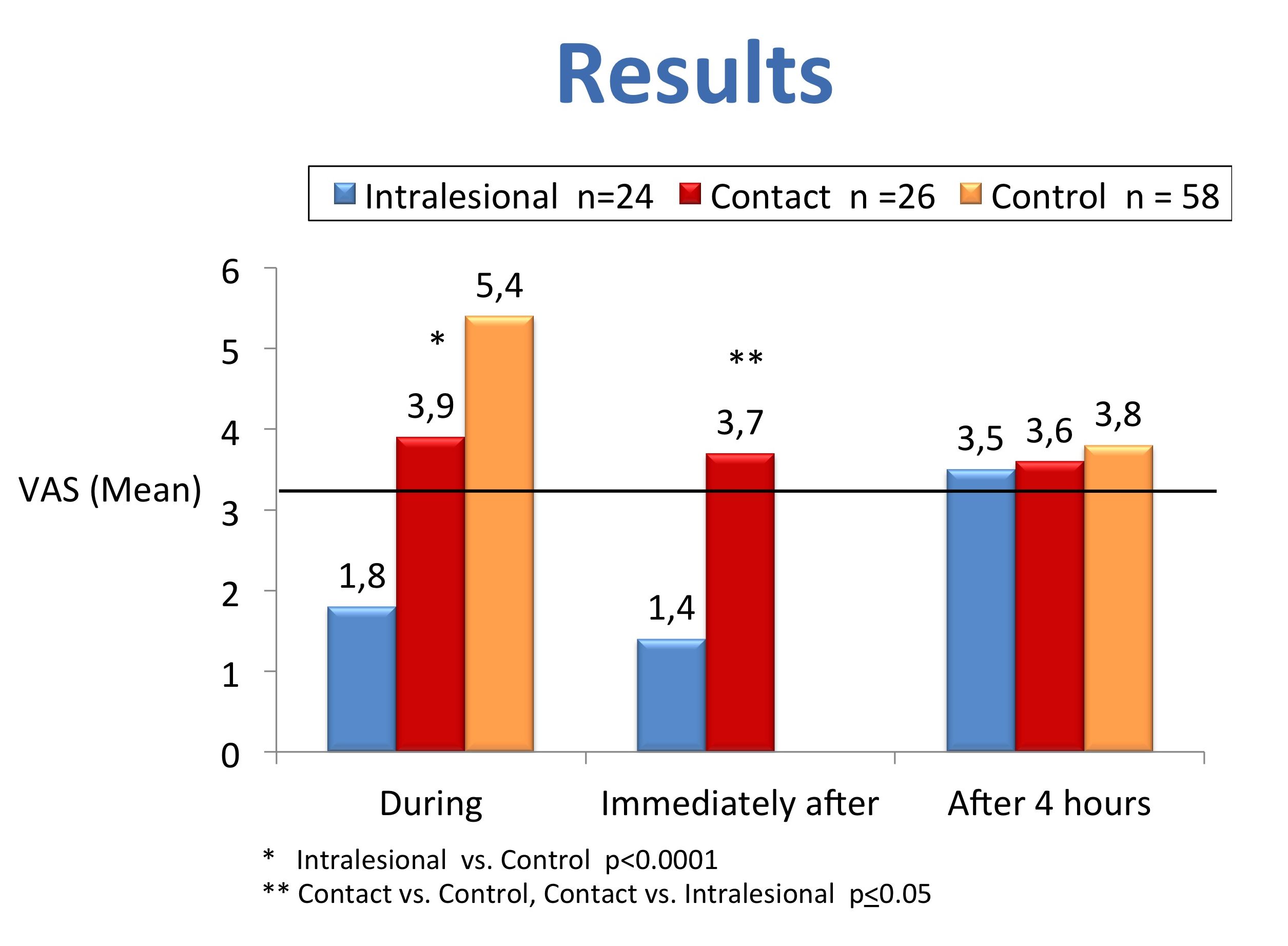
The lethal temperature zone (Fig. 1) is so low that all pathological tissue cells can be destroyed. At the surface, however, the temperature is not so low that the melanocytes survive the treatment. This prevents permanent depigmentation. No damage was found in the healthy tissue. The reason for this is the good blood circulation of the healthy tissue compared to the keloid, which prevents a critical temperature reduction. Compared to contact or spray cryosurgery, patient acceptance is considerably better. The pain sensation during the treatment is lower, after approx. 4 hours the pain of all cryotherapy methods is approximately identical, but then it can be well tolerated by almost all patients (Fig. 2).
The reduction of the keloid volume depends on the localization. Most keloids are located in the ear area or on the chest and shoulders. At the ears the volume reduction can reach 70 %, at the body 50 to 60 %.
The most important criterion for the acceptance of the therapy is the recurrence rate. While all other therapies for the treatment of keloids have to calculate with recurrence rates of 40 to 70 %, intralesional cryosurgery this is 5 to 7 % in a follow-up period of seven years. Further studies were published last year. A working group from Aachen has investigated the improvement of the results by combining intralesional cryotherapy and silicone patches. A French and an Egyptian working group submitted larger patient numbers validating the results reported by Har-Shai and others.
Bibliography alphabetically by authors
Abdel-Meguid A M, Weshahy A H, Sayed D S, Refaiy A E M, Awad S M I: Intralesional vs. contact cryosurgery in treatment of keloids: a clinical and immunohistochemical study, DOI: 10.1111/ijd.12667
Chopinaud M, Pham A, Labbé D, Verneuil L, Gourio C, Bénateau H, Dompmartin A: Intralesional Cryosurgery to Treat Keloid Scars: Results from a Retrospective Study
in: Dermatology ,DOI: 10.1159/000365392, September 2014
Dalkowski A, Schuppan D,.Orfanos Çñ C E and Zouboulis C C: Increased expression of tenascin C by keloids in vivo and in vitro, British Journal of Dermatology 1999; 141, 50-56
Dalkowski A, Fimmel S, Beutler C and Zouboulis C C: Cryotherapy modifies synthetic activity and differentiation of keloidal fibroblasts in vitro, Experimental Dermatology 2003: 12: 673–681
Har-Shai Y, I Mettanes, Y Zilberstein, O Genin, I Spector, M Pines: Keloid histopathology after intralesional cryosurgery treatment, JEADV, DOI: 10.1111/j.1468-3083.2010.03911
Har-Shai Y, Brown W, Labbé D, Dompmartin A, Goldine I, Gil T, Mettanes I and Pallua N: Intralesional Cryosurgery for the Treatment of Hypertrophic Scars and Keloids Following Aesthetic Surgery: The Results of a Prospective Observational Study, The International Journal of Lower Extremity Wounds, 2008; 7; 169, DOI: 10.1177/1534734608322813
Har-Shai Y, Amar M, Sabo E: Intralesional Cryotherapy for Enhancing the Involution of Hypertrophic Scars and Keloids, PRSJ Vol. 111, No. 6, 2010, 1841-1852, DOI: 10.1097/01.PRS.0000056868.42679.05
Har-Shai Y, E Dujovny, E Rohde, CC Zouboulis: Effect of skin surface temperature on skin pigmentation during contact and intralesional cryosurgery of keloids, JEADV 2007, 21, 191–198
Har-Shai Y, Sabo E, Rohde E, Hyams M, Assaf C, Zouboulis C C: Intralesional cryosurgery enhances the involution of recalcitrant auricular keloids: a new clinical approach supported by experimental studies, Wound Rep Reg (2006) 14 18–27, DOI:10.1111/j.1743-6109.2005.00084
Har-Shai Y und Weidmann M: Die Behandlung von Keloiden und hypertrophen Narben durch intraläsionale Kryotherapie, Kosmetische Medizin 2.12, S. 4-8
Har-Shai Y, Amar M, Sabo E. Intralesional cryotherapy for enhancing the involution of hypertrophic scars and keloids. Plast Reconstr Surg 2003; 111: 1841–1852.
Har-Shai Y, Sabo E, Rohde E et al. Intralesional cryosurgery enhances the involution of recalcitrant auricular keloids: a new clinical approach supported by experimental studies. Wound Repair Regen 2006; 14:
18–27. Erratum in: Wound Repair Regen 2007; 15: 163.
Har-Shai Y, Brown W, Labbe´ D et al. Intralesional cryosurgery for the treatment of hypertrophic scars and keloids following aesthetic surgery: the results of a prospective observational study. Int J Low Extrem Wounds 2008; 7: 169–175.
Har-Shai Y, Har-Shai L:Intralesional cryosurgery for the treatment of upper lip keloid following deep chemical peeling; Eur J Plast Surg DOI 10.1007/s00238-014-1016-7
Mende B. Keloid Behandlung mittels Kryotherapie. Z Hautkr 1987; 62: 1348–1355.
Mirmovich O, Gil T, Goldin I, Lavi I, Mettanes I, Har-Shai Y: Pain evaluation and control during and following the treatment of hypertrophic scars and keloids by contact and intralesional cryosurgery – a preliminary study, JEADV 2011, DOI: 10.1111/j.1468-3083.2011.04092.
Weidmann M: Keloide und hypertrophe Narben mit intraläsionaler Kryotherapie behandeln, Ärztliches Journal Reise und Medizin 7-8, 2012, S. 6-7
Weidmann M: Intraläsionale Kryochirurgie zur Keloidbehandlung, Spitzenforschung Ästhetische Dermatologie und Dermatochirurgie, Jahresheft 2016, 66 + 67.
Rusciani L, Rosse G, Bono R: Use of cryotherapy in the treatment of keloids. J Dermatol Surg Oncol 1993; 19: 529–534.
Seifert O, Mrowietz U: Keloid scarring: bench and bedside. Arch Dermatol Res 2009; 301: 259–272.
Stromps, JP; Dunda, S; Eppstein, RJ; More: Intralesional Cryosurgery Combined With Topical Silicone Gel Sheeting for the Treatment of Refractory Keloids Dermatologic Surgery. 40(9):996-1003, September 2014.
Stromps JP, Kolios G, Cedidi C. Atiyeh BS, Costagliola M, Hayek SN.: Intralesional Cryosurgery Combined With Topical Silicone Gel Sheeting for the Hypertrophic scar and keloid formation after male circumcision. Keloid or hypertrophic scar: the controversy: review of the literature. Ann Plast Surg 2005; 54: 676–680.
Zouboulis CC, Orfamos CE. Kryochirurgische Behandlung von Hypertrophen Narben und Keloiden. Hautarzt 1990; 41: 683–688.
Zouboulis CC, Blume V, Buttner P, Orfanos CE: Outcomes of cryosurgery in keloids and hypertrophic scars: a prospective consecutive trial of case series. Arch Dermatol 1993; 129: 1146–1151.
Zouboulis C C et al.: Modification of a Device and Ist Application for Intralesional Cryosurgery of Old Recalcitrant Keloids, Arch. Derm. Vol 140, Oct. 2004
Zouboulis C C: Principles of Cutaneous Cryosurgery: An Update, Dermatology 1999;198:111–117
Zouboulis C C: Cryosurgery in dermatology, Eur J Dermatol 1998; 8: 466-74
Zouboulis C C, Zouridaki E, Rosenberger A, Dalkowski A: Current developments and uses of cryosurgery in the treatment of keloids and hypertrophic scars, Wound Repair And Regeneration, March-April 2002, 98-102
Scar-Council
The Faculty of Keloid has determined that there is a great need on the part of our colleagues and also on the part of patients for a contact point for the subject of scars. With the Scar Council we have created a body that wants to give this support.
The Scar Council deals with all new developments for the prevention and treatment of all types of scars.
We would like to invite colleagues who are involved in this issue to participate in this panel.